News Feed › Discussions › 25 Months since Dr. Brown permanently release my entire abdominal wall
-
25 Months since Dr. Brown permanently release my entire abdominal wall
Posted by PeterC on March 9, 2022 at 6:54 amHey ya’ll its me again. Yesterday marked 25 months since Dr. Brown permanently released my external obliques and by extension my entire abdominal wall. Picture on the left was me my entire life/before Dr. Brown operated on me and picture on the right was taken 5 minutes ago after 25 months of attempted conditioning.
What you guys can’t see just looking at the picture is that by releasing my abdominal wall permanently it weakened/released tension in tissues across my entire body.
I have erectile dysfunction, ejaculatory dysfunction, the muscles between my ribs and all the way up to my pectorals completely released, my back muscles, my leg muscles are dysfunctional (everything that attaches to the illiac crest is weak), my feet aren’t aligned anymore when I walk because of that chain-reaction of tension loss.
Its been 25 months of doing conditioning, abdominal exercises every single day. As you can tell by the picture, the tissues dont work anymore. They cannot be conditioned. What Dr. Brown did to me is the equivalent of someone slicing your achille’s tendon and cutting parts out of it that he then reattaches in random places and then asking you to walk properly on that leg or go back to sports.
This is what happens when general surgeons with private practices are trying to find new avenues to generate income and start doing procedures they are not qualified to do on parts of the body they clearly do not understand – all to make money. Money is apparently more important than a whole human life.
Mind you when I agreed to this surgery with Dr. Brown I explicitely told him my entire career is on the line, that I’m a professional dancer in L.A, that it took me over a decade to get to where I’m at, and asked him if there was ANY CHANCE of permanent weakness or dysfunction as I could not afford that chance. I flew my parents out to meet him and he also assured them that it was safe.
I also asked if it could affect my genitalia or sexual function in any way and he said absolutely not then proceeded to dissect my spermatic cord on both sides for no reason when I was on the operating table evn though he had never brought this up, I had no testicular or spermatic cord symptoms at all.I’m posting this for awareness – I want people to see this. I did everything right, I asked all the right questions, I was on the healthiest diet possible, I prehabbed with an olympic athletic therapist to shorten recovery time and I put my trust in a doctor who lied directly to my face and proceeded to butcher me to the point of permanent dysfunction. I can’t even get it fixed the damage has been done the tissues will never work again even if someone goes in to undo the atrocity he did and puts the muscles back into 1 piece.
I lost my career, my life and even my friends because I feel too much shame to even talk to anyone. How do you explain that you went to see a doctor for help with an overuse injury and you walked out completely disfigured with permanent weakness and sexual dysfunction and that you most likely will never be able to do sports or have kids? How does one even begin to recover from the mental and physical trauma?
Be careful out there.
Watchful replied 3 years, 11 months ago 5 Members · 21 Replies -
21 Replies
-
Mike M… Sounds like you’re going to have it done by Dr. Kang. Let us know how it goes. I think a number of people here are thinking about doing the same thing, including me.
-
Dr. Grishkan’s philosophy expressed to me was if the inguinal floor is damaged then the floor is damaged. I think he takes the position to fix everything so it is bulletproof.
Dr. Grischkan caters to a lot of powerlifters so maybe it makes sense.
I know if you have a small hernia there would be an option to not use the goretex repair with Dr. Grishkan.
I am debating which route to go regarding sutures. Absorbable, prolene, goretex, etc. I am pretty sure Dr. Kang can do all the above if requested. I guess when I finally see how big and bad my hernia is I will see what Dr. Kang recommends.
I dont weightlift as much as I used to but I do chop wood and toss 100lb logs around all day long in the summer “for fun” on one of my horse ranches. I also have to manipulate 2000lb+ Clydesdales when they get lively. Finally I am closer to 50 now than 40. Like GI mentioned I do have concerns as it relates to collagen rehab time regardless of any procedure.
I have had this hernia known for 6 weeks. Sometimes it comes after me in a blaze of glory and other times I just barely notice it is there. Either way 2 weeks from now it will be gone and hopefully for good.
-
Is there surgery that isn’t major? The body didn’t evolve in a way that’s friendly to repairs by surgeons, unfortunately.
The 4 days isn’t the major issue there. The major one is not being able to choose the surgeon. Then there’s the removal of the cremaster and cutting of the genital nerve branch.
In general, the Shouldice procedure seems a bit excessive for an indirect inguinal hernia, which is the reason surgeons are trying simpler, less radical approaches, such as Kang (modified Marcy, I guess) and Desarda. Based on my interaction with the few US tissue repair surgeons who offer Shouldice, they offer it a bit reluctantly, and try to steer you away from it. That bothers me a bit. The only exception is Dr. Sbayi.
-
I’m just trying to add a perspective. As for the four days…if you have problems four days will seem like just a moment, a faint memory, that you wished you had spent. It’s very hard to get the point across to people planning for hernia repair that even though the procedure can be quick and seemingly simple, the results last for the rest of your life. The surgeon won’t feel it but the patient will.
Posting this made me realize that words like “major” or “minor” are meant for the surgeon on the day of surgery. But really they should use the words to describe the impact on the patient. Hernia repair is major surgery.
-
It’s based on what they say – I actually asked them. You can’t do much more than that for verification of what you’re going to get, other than maybe go to the Shouldice Hospital, but that has its issues too. Maybe you can be more certain that you will get the exact procedure, but how well it’s performed depends on the surgeon you end up getting, there’s the cremaster/nerve issue, old-school closure of the incision with metal clips, and who wants to stay there for 4 days…
-
“They adhere to the original (other than the steel sutures) ”
My point was if you don’t know the details you don’t know the modification. Dr. Grischkan used the word “modified”. Who really knows what those three, or anyone, are doing, if they changed the sutures maybe they thought something else wasn’t quite right. A small mod here, a small mod there…it doesn’t take much and you have a whole new technique. Two layer Shouldice was probably considered modified Shouldice, maybe it still is. If you read about why permanent sutures are used, because new collagen takes months or years to reach full strength, then even absorbable sutures are not “true” Shouldice.
Dr. Kang proposed that much of the bad press for pure tissue repairs has come from “modified” Bassini techniques being used. People see “Bassini” but it’s not really Bassini, it’s something else. Really, if it’s modified it shouldn’t even have the originators name behind it.
The same is true, maybe especially true, for mesh. Lichtenstein paved the way, and the people that have followed have exploited that for all that they can get. All kinds of crazy combinations of materials, even food supplement coated mesh materials, have been extended out from Liechtenstein’s work through the 510(k) procedure. Just because it’s different, AKA modified, doesn’t mean it’s better. Be careful what qualities you’re ascribing to these modified procedures.
-
This Goretex mesh surgery is pretty far from Shouldice. I was referring to the modification by Yunis, Reinhorn, Towfigh, etc. They adhere to the original (other than the steel sutures) There’s no mesh, and they leave the cremaster and its nerve.
-
If there is no name associated with the word “modified” then modified just means different. For example, Grischkan’s modified Shouldice is a version of the Shouldice procedure but with a piece of Gore mesh, and other differences, as the modification.
https://www.herniasurgeries.com/modified/
And, as this old thread seems to show, the details get lost as the modifications are described. Like the telephone game.
https://herniatalk.com/forums/topic/dr-grischkan-modified-shouldice-technique/
-
These discussions about the fine details of the repair techniques are interesting, but, in the end, I think, the results are what matter.
If you want to extend the understanding over to mesh repairs then you should consider the peritoneum, the omentum, the fascia, and muscles and ligaments that get pulled as the mesh (actually mesh/tissue composite) shrinks. Omentum is often one of the materials that gets pushed through a hernia. The omentum is actually a folded portion of peritoneum. It is considered as an organ of the body.
Here is a good starting point for the peritoneum and the omentum. These parts of the body are involved in the foreign body response to the mesh. More mesh contact probably means more response, a person would guess.
https://www.frontiersin.org/articles/10.3389/fphys.2018.00738/full
A couple of excerpts –
“Background: Despite its complexity, the peritoneum is usually underestimated in classical medical texts simply as the surrounding tissue (serous membrane) of the gut.”
“Nonetheless, peritoneal cavity is usually disregarded as an empty space without clear clinical significance (Sasaki, 1999) and the peritoneum simply as the covering tissue (serous membrane) of abdominal viscera in classic physiology (Hall and Guyton, 2015; Boron and Boulpaep, 2017), and histology texts (Ross and Pawlina, 2012).”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723480/
Excerpt –
“A more conventional view of the omentum is that it plays a central role in peritoneal defence by adhering to sites of inflammation, absorbing bacteria and other contaminants, and providing leukocytes for a local immune response[3]. This review details current knowledge on the origins, structure, and function of the omentum, and discusses its role in the peritoneal cavity during various disease states.”
-
That was one of my biggest questions.
Does the Cremaster still function after being cut / shaved / modified etc?
Cremaster is Skeletal muscle and when damaged these cells are stimulated to divide. The division process causes the cells to fuse with *existing* muscle fibers. The Muscle fibers regenerate and repair the damaged fibers.
The skeletal muscle fibers themselves, cannot divide *after birth. However, muscle fibers can lay down new protein and enlarge (hypertrophy).
So you have a few things at play here.
#1. If you take 30%-50% of the Cremaster you are causing some permanent damage in the sense the muscle fibers aren’t able to divide and just “poof” restore the muscle that is now missing. However the fibers that remain are getting a “work out” and can enlarge to potentially maintain the same muscle function as before because they will grow and increase in size / strength? At least as I understand it.
#2. Dr. Kang method appears to cause injury but he isn’t actually ***removing*** muscle tissue thus any damage incurred should be superficial. Skeletal muscle is designed to react and *HEAL* completely to the damage that Dr. Kang is causing in his procedure to the Cremaster muscle. At least how I understand it.
IMHO – “Cut through” and/or “Remove” healthy tissue / nerves, etc is a very very bad thing especially in this procedure.
It would be nice for one of the medical experts to chime in and correct me if needed and add input.
-
MarkT… That’s great. Did they give you surgical notes? Do they say that they cut the cremaster muscle and genital nerve branch?
More importantly, how are your repairs holding up? Any long-term pain, discomfort, or other issues?
-
Not to stray too far from the OP, but it is worth noting that the way the cremaster is treated during some repairs does not mean you will lose the cremaster reflex.
I’ve had right side (30yrs ago) and left side (18yrs ago) inguinal hernia repairs done at Shouldice, and the cremaster reflex is still present.
-
Mike M… The Shouldice Clinic cuts the muscle and the nerve, and so does Dr. Sbayi. I believe this is regardless of whether the hernia is direct or indirect. My understanding is that they need to do it to visualize and access the entire area, not just for the tighter repair.
If I remember correctly, Dr. Kang said that he does some minimal cutting of the cremaster in his procedure.
I read that Dr. Grischkan shaves the muscle by 50%, but doesn’t cut the nerve.
Dr. Yunis supposedly keeps both the muscle and the nerve intact. I don’t think he has some special method to avoid this. It’s basically a simplification of the procedure where you are willing to sacrifice one thing for another – there’s a tradeoff there. Keeping the cremaster/nerve, but possibly having a higher recurrence rate (as shown in some studies of this), and maybe not doing as thorough a repair because the cremaster gets in the way. This is just my understanding as a lay person based on reading – I’m not a surgeon or expert on this.
By the way, based on a discussion I had with Dr. Brown, cutting the cremaster and its nerve wasn’t a part of his standard procedure, but maybe he did that in the case of PeterC for some reason. He wasn’t going to do it in my case of an indirect inguinal hernia. I ended up not going with him because his combo procedure of both Shouldice and Desarda seemed like overkill to me. However, maybe this is the reason he could get away with not cutting the cremaster while still minimizing recurrence – he was strengthening the repair with the Desarda.
-
The cremaster muscle is the thin fascial muscle of the spermatic cord made of skeletal muscle.
Indirect hernia you have to deal with it in terms of manipulating it more surgically (shaving possibly for a tighter repair) because it drops through the ring which is where the hernia occurs? Dr. Kang and Dr. Yunis have another method that avoids this potentially unfortunate step? None of the doctors I spoke to including Dr. Grischkan cut any nerves. Dr. Yunis had stated to another member that “no one does that anymore?” but I am sure some still do. Perhaps the Shouldice Hospital?
One of the members on here had it down at the Shouldice Hospital and stated he didn’t realize they did that or know a difference before/after?
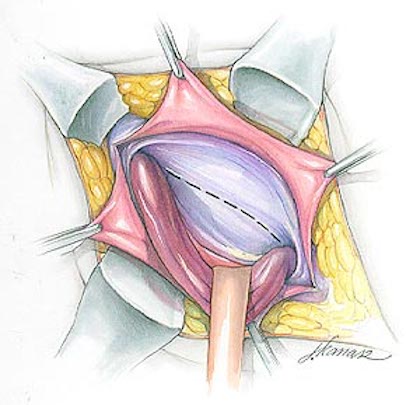
If the procedure only deals with direct I would think it just needs to be moved out of the way as illustrated.
-
Mike M… I’m not a surgeon, but my understanding is that the cremaster muscle is part of the cord, and it is sometimes dissected, or “shaved”, etc. in tissue repair procedures. The genital nerve branch is there as well, and it is cut in the Shouldice procedure (at least the original one).
-
First let me say I am very sorry to hear that this happened to you and I hope you can find someone to resolve your problems long term.
@Herniatalk Community Regarding “dissect” the spermatic cord w/ open tissue repair.
Doesn’t almost every open tissue repair require this procedure and it simply means you are carefully moving the cord out of the field of surgery for direct hernias moving it back in place once it is completed?
I assume this is to prevent damage during the actual repair of the hernia itself?
-
Mike M… I think the modification in the “modified Shouldice” is simply that the cremaster muscle and the genital nerve branch aren’t cut. I don’t believe they do anything to eliminate the need for this – they just don’t do this part. There’s a tradeoff there, and whether it’s a good or bad tradeoff is controversial – there’s no consensus on that among surgeons.
-
@MarkT – The vast number of successful and documented repairs of Shouldice (and modified) is the biggest selling point. Follow up from you and others that have experienced it with success (including no loss of cremaster function) is a testament that there are other viable options out there besides the status quo mesh mesh mesh.
I think the point to being so hyper focused on one aspect or another for a particular procedure is solve these concerns. Can we dismiss it ? or it is really an issue? There is a lot of mixed opinions so the more successful input the better.
I have a lot of respect for surgeons like Dr. Kang, Dr. Grischkan, and Dr. Yunis who continue to modify and improve sound methods by reducing the amount of the nerves, tissue, and overall area impacted.
It is my understanding that Drtowfigh has also created innovations and vast improvements for the mesh procedures that she performs?
I think mesh has its place too. If I was 65+ or had a pre-existing condition (connective tissue disorder like marfans? perhaps) someone could probably convince me to pick mesh over an open tissue repair. There have been countless numbers of “successful” mesh repairs without issue. I am not a fan of it because of how the operation is performed and the underlying requirement of mesh to ultimately solve the problem at my age. Since there are other viable options available I will pick just about any other route.
@Good Intentions – Outside of the usual negative stories of mesh it is interesting to get more details regarding of what mesh modifies / interacts with in that area. I wonder how the other open “pure tissue repair” materials break down and/or interact with that area over time. There seems to be a lot of material options open tissue repair doctors use from flexible gore-tex to ones that dissolve over time.
-
It is worth bearing in mind that the Shouldice repair has a long history behind it…50+ years and hundreds of thousands of total repairs.
Do we have any evidence, even anecdotally, that the way the cremaster is treated carries a relatively high level of risk for negative outcomes? And that this risk is not offset or more than offset by the benefits of treating it they way they do? Wouldn’t we have many thousands of Shouldice patients with low or non-functioning cremaster reflex (or other negative outcomes) that would have identified this aspect of the repair as a key concern?
Of course I would rather see data than hypothesize in this manner. My point is not that the cremaster dissection is a ‘trivial’ concern…I just question whether it should be a *key* concern or barrier when making a decision on repair type.
-
Glad to hear your repair is holding up so well after all these years – that is awesome.
The cremaster keeps coming up because it’s a controversial part of the procedure. Some surgeons don’t believe in doing it. Also, patients tend to prefer not to have a muscle and nerve cut if not necessary. Some people do complain about a low hanging testicle after this. Also, some sensation is lost in the scrotum, although supposedly this comes back eventually, maybe because other nerves compensate.
-
Watchful, I don’t have notes, so I can’t confirm with certainty, but dissection of the cremaster is apparently standard procedure at Shouldice Hospital, so I can’t imagine that mine wasn’t touched in two repairs by different surgeons? I suppose I could try to get notes though…I was actually there very recently and completely forgot to ask about cremaster, since that keeps coming up here as a concern (I don’t really know why) by people contemplating repair options.
Zero complications or chronic pain after both repairs and no restriction whatsoever on lifestyle (weights, swimming, yoga, etc) since then.
Long story made short, I severely overstretched abs/groin/thighs this past September and thought I had a new hernia or recurrence…but multiple doc visits, ultrasound and CT, and a very recent visit to Shouldice for exam by two different docs, has yielded no evidence of a hernia. Shouldice doc believes it to be adductor insertion strain that keeps getting aggravated before properly healing, so I’m treating it as such for now.
I am hoping to get an MRI at some point to confirm a diagnosis of some kind, but the backlog following the pandemic means waiting until at least April for an appt…
Log in to reply.
