News Feed › Discussions › Healing from mesh removal surgery
Tagged: bard soft mesh, billing, mesh removal, recovery
-
Healing from mesh removal surgery
Posted by Good intentions on June 28, 2021 at 5:33 pmajm22 expressed interest in my healing from mesh removal surgery, about 3 1/2 years ago.
I kept a log, with entries almost every day, from 12 6 2017 to 5 23 2109. Looking back through the entries, it’s basically a long series of ups and downs. Feeling good, then feeling healing pains again. At times, even one full year later, I was wondering if indirect hernias were forming. There was often a feeling of pressure in the inguinal area, with gurgling and a feeling of peristalsis. But, as far as I know, no hernias have formed. So I spent a lot of time wondering, over the course of a year or more, if I was going to have to have more hernia surgery, even drafting a letter to Dr. Brown at one year after the mesh was removed. That’s how bad it was. But, no hernias today, 3 1/2 years later.
While I was healing I was pretty active. Lots of running and light weight workouts and working around the house. One of my concerns was that since the peritoneum had been peeled off of my abdominal wall from hip bone to hip bone and navel to pubic bone, that the area would heal in a constricted fashion. There is essentially zero advice out there about how to heal from such a thing. Lots of focus on the incisions, but not much on the burned battlefield left behind from the cauterizing tool.
I did find that sometimes rest was not a remedy for pain. Exercise was. Based on Dr. Bendavid’s theory of “toxic zones” around the tissue that grows in to mesh, I would often go out for rigorous exercise after a few days of waiting for pain to resolve. It helped a lot.
There were a few times when it felt like something had pulled free, like an adhesion or something that was where it was not supposed to be. All I could do then was wait and see if things got worse.
At this point, the spot where the mesh remnant is, on the right side, still gets sore after long walks. But the rest of the damaged area seems to have recovered, except that I still feel like I have a plastic bowl in my lower abdomen. But it’s getting more and more flexible as time goes on.
When the mesh was removed Dr. Billing found that it was surrounded by edema. Basically the tissue around the mesh was in constant damage/repair mode. I would guess that I have a thick layer of tissue wherever the mesh was in contact due to the constant healing process. After three years that could be a lot of excess tissue. People who have mesh removed early might not have that.
I tried to create a more consistent and cohesive story but it really was just a long series of 2, 3 and 4 day projects. Try to define a base, try some activities, monitor results, adjust the plan and start again. Suffer, and hope, through the times when you had to get things done despite the pains.
I hope this helps anyone who was expecting a rapid months-only long healing process. My notes say that Dr. Brown found that it took about 9 months to get back to feeling normal and Dr. Billing said 1 1/2 to 2 years. That’s probably open versus laparoscopic, and small pieces of mesh versus large, respectively.
Mesh removal, by its nature, requires creating more damage to get the mesh back out. What’s left behind takes time to be repaired.
Good intentions replied 1 month, 2 weeks ago 10 Members · 48 Replies -
48 Replies
-
Realized a minor milestone today. I can wear my old 34 inch waist shorts without pain or discomfort. I had almost given them away since even a 36 inch waist had been uncomfortable. I never thought that my abdomen, the mesh damage zone, would feel right again.
The list of little tricks I developed over the years have all helped. I’ve increased the level of exertion in my exercise and the duration and have taken up running again. The consistent progress, although taking years, shows that it was the mesh that did most of the damage. My abdominal wall seemed to have thickened, and the remnant of mesh that was left behind was still causing pain and localized inflammation. I can still feel it at times but it doesn’t seem to affect as large of an area as it did.
Posting for anyone that is still trying to recover from mesh removal. If things got bad enough to have the mesh removed then the damage that was caused will probably take years to heal and readjust. Don’t lose hope. Just keep working at it. It really is a shame that the community of surgeons has given up trying to find a better hernia repair method.
But the gaslighting, or outright ignorance, continues. It’s pretty amazing.
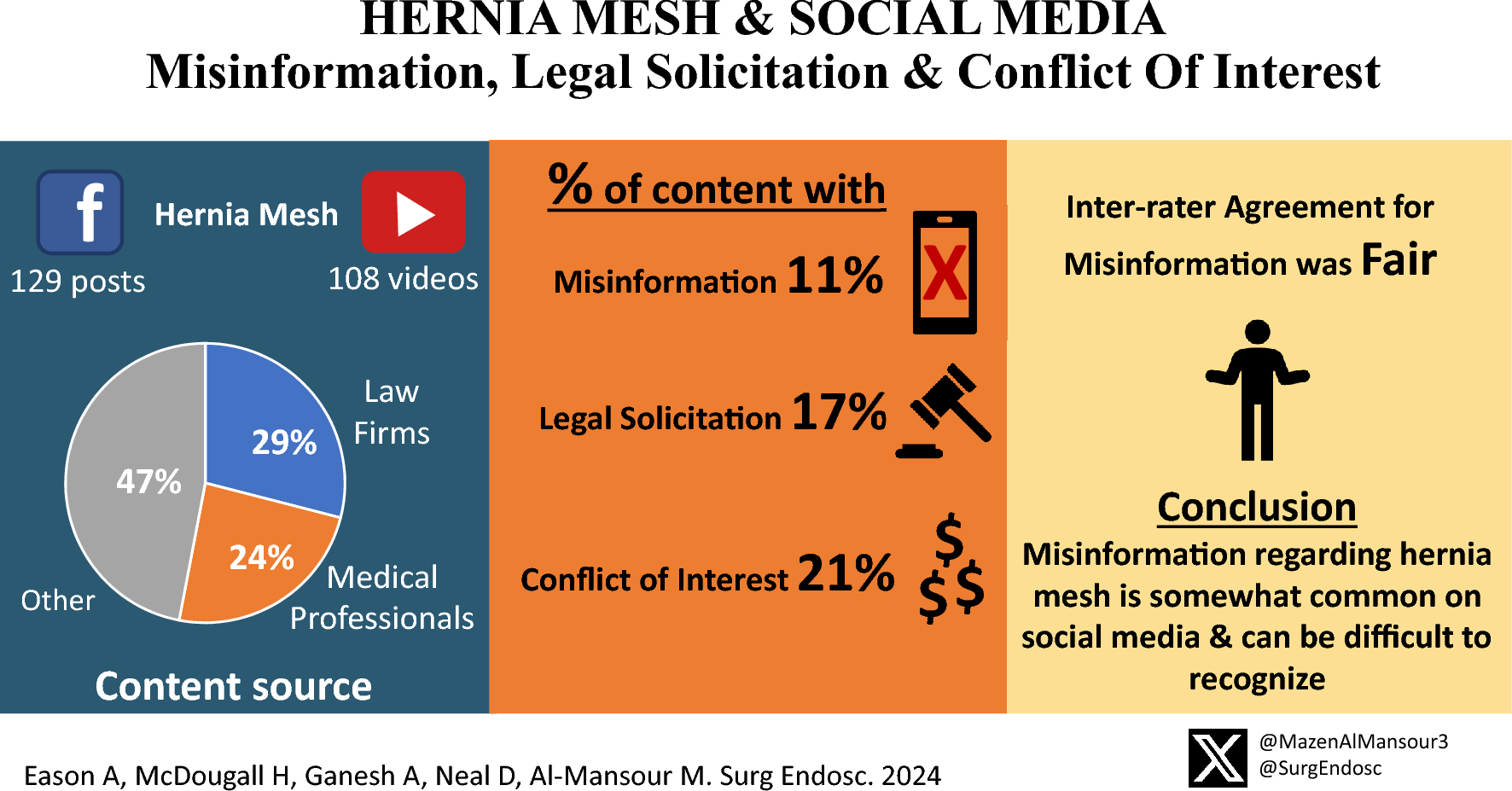
https://link.springer.com/article/10.1007/s00464-024-11320-w
link.springer.com
Background Patients often utilize social media platforms as a resource for medical information. Lately, hernia mesh has been surrounded by controversy due to highly publicized mesh recalls. We aimed to assess the rates of misinformation, legal solicitation, and conflict of … Continue reading
-
Hello GI, thank you for sharing your story, I’ve been thinking of removal of the 2 meshes planted in 6 months last year and this year. I thank you from my heart that anyone recommend experience surgeons in mesh removal in greater Los Angeles.
-
No idea where this post will end up, there is still no way to ensure that a post will appear at the end of the thread, like in a normal forum. It’s kind of disturbing that Dr. Towfigh refuses to acknowledge this. It makes you wonder about resistance to improvement. But, I think it’s still worth adding to the thread for anyone stuck in the early phases of mesh damage. There is hope for recovery, but it can take a long time.
I’ve posted over the years about the slow progress in recovering from the damage that the mesh implants did, after having them removed and trying to recover. I’ve found that a person’s main hope is to just become an expert in how their own body responds to their activities, and the clothes that they wear, and the length of time they need to wait when things get bad. It requires a continuous cycle of ups and downs, a sort of saw-tooth pattern, slowly rising, but with regular periods of pain and soreness along the way. I have an advanced degree in a field which is very logic and experimentation oriented and I still had to work extra hard to figure out how to heal myself. It is incredible to me that I allowed myself to get fooled in the beginning (I wanted to believe), and that the mesh could cause so much damage. But, also, incredible that the body will continue to try to get back to normal function if allowed to.
At this point in time the site of the mesh damage responds about like a normal body part would. Like a heel that gets sore if you walk too far in tight shoes, or an area that chafes if your clothes are too tight over an extended period. There is soreness and pain but it dissipates overnight or within a day or two. I am capable of wearing my old properly fitting pants now, looking like a normal person instead of somebody wearing pants two inches too big in the waist. I can plan for a whole day without worrying about taking a day or two off afterward to recover. I am back to living a normal life, without taking care of my damaged abdomen on a daily basis.
It is coming up on ten years since I had the mesh implanted. Seven years since I had it removed. It’s a shame that this in-and-out one hour mesh implantation has damaged ten years of my life, along with damaging the lives of family members that counted on me to be available for them. But it’s the world we live in today. The device makers continue to sell the bad products, the monetary legal damages are factored in to the costs of operation, and the surgeons are stuck implanting these poor devices, knowing that they are damaging 15 to 20 percent, at least, of their patients. Damaging the surgeons themselves in the process.
All for the money.
Good luck to the fellow sufferers. Don’t give up.
-
Hi I’m a 36 year old male I want our story heard since this is the only media outlet where others like myself can speak to one another and it’s time we get together for ourselves and any future victims. That being said here is my story. I was really active fit enjoy all sorts of physical activities. I was a medic in the military with 2 deployments fitness trainer did mma and due to complications my whole life has been stolen from. Since 2015 I’ve had 10 surgeries causing me to lose both testicles leaving me urinary incontinent and now facing a 11th procedure in the future. Due to mesh. It has effected many aspects of my life from employment sex to every day activities. Worse of all my ability to get my son back in my life cause I’m having to take so much time for recovery. I think it’s time the doctors hospitals and companies take responsibility for the damage the mass tort cases only benefit the lawyers and the company by forcing to take the small settlement offered. Not one of us has had a say of any kind throughout the proceedings mostly radio silence and all I get from my lawyer at parker waichman is this how it’s done sad how you get better representation as a criminal I’m currently being offered 67000$ no help with medical or reoccurring costs each month and given the company earnings the entire settlement is just a slap on the wrist so if there are others out there like me please reach out they’re still using mesh and it could be your child in the future let’s end it now enough is enough
-
I feel compelled to add another comment about doing whatever it takes to remove pressure on the outside of the hernia repair area. Since getting rid of tight waistlines on pants and belts, and using suspenders to hold my pants up instead, I have really been able to get back closer to my old self. More strenuous running and able to to work harder, without needing to rest for a day or two in between. So much so that “taking care of the damaged hernia repair area” is no longer my primary thought to start, and during, the day. I hadn’t realized how much of my thinking time it was occupying until I didn’t need to think about it anymore.
The weather has warmed up and I put on a pair of shorts with a tight waistband and felt the old discomfort creeping back in almost immediately. Trying to be “normal” had really been holding me back. Suspenders have made a huge difference.
Anyway, it’s something to try if you’re having pain or discomfort after a hernia repair or mesh removal.
I will post this separately as an Update since my last post got buried in the thread. It was the last chronologically but it got placed somewhere up above.
-
Not sure what’s happening, the software showed my double post as being at the end of the thread then moved it up a few again. Anyway, if this is at the end, scroll up a few posts and check the date. Good luck people.
-
This will be a double reply. I used the red “Reply” button at the upper right and the software stuck my reply in to the middle of the stream. I assume, maybe, wherever my cursor was.
Hopefully this one shows up at the end of the thread where it can be found, as I thought it would.
Might as well give the forum software some more testing. It is now almost six years since I had mesh removed by Dr. Billing of Transform Weight Loss in Kirkland Washington. Things have been going very well, My range and duration of activities is still slowly expanding. I don’t really have any “down” days anymore, every day is open to spontaneous possibilities. Lifting heavy weights, walking long distances, running, sprinting. I do still get some soreness at the spot of the original hernia, but it feels like it is generated from the outside now. From slight constant external pressure on the spot.
So, as I’ve said before, I don’t want to make anyone feel bad about the long time it might take to get back to full fitness, six years is a long time. But I’d also like to give some hope to people that expected faster results from their surgery, whether it was mesh removal or hernia repair, if recovery is slow for them If you’re feeling progress it will probably continue.
But, also, to be clear, as far as mesh repair surgery, I was making zero progress of recovering from the original best practice top level best surgeon standard of care of TEP implantation of Bard lightweight Soft Mesh. My first ever surgery of any kind was a disaster that lasted three years plus the years after to heal from mesh removal So if you’re having mesh problems don’t let this account convince you to wait too long. You’ll know if things have any chance of getting better.
Also, finally, and maybe most importantly, Dr. Billing really does seem to know what he’s doing “in there”. If you’ve watched any videos of surgeons narrating what they’re doing and/or heard them describe it, there are all sorts of different ways that surgeons do things. There is no standard practice mesh removal method. As far as I know and according to his surgery notes, all that he did was carefully remove as much mesh as he could. No neurectomies were noted as having been done and I do not have any symptoms of neurectomy. No numbness or phantom pain. And no signs of recurrence.
So I can sincerely recommend seeking out Dr. Billing if you feel that you need to have mesh removed.
-
Double post. The software placed my reply in the middle of the thread. I copied it to the end.
Might as well give the forum software some more testing. It is now almost six years since I had mesh removed by Dr. Billing of Transform Weight Loss in Kirkland Washington. Things have been going very well, My range and duration of activities is still slowly expanding. I don’t really have any “down” days anymore, every day is open to spontaneous possibilities. Lifting heavy weights, walking long distances, running, sprinting. I do still get some soreness at the spot of the original hernia, but it feels like it is generated from the outside now. From slight constant external pressure on the spot.
So, as I’ve said before, I don’t want to make anyone feel bad about the long time it might take to get back to full fitness, six years is a long time. But I’d also like to give some hope to people that expected faster results from their surgery, whether it was mesh removal or hernia repair, if recovery is slow for them If you’re feeling progress it will probably continue.
But, also, to be clear, as far as mesh repair surgery, I was making zero progress of recovering from the original best practice top level best surgeon standard of care of TEP implantation of Bard lightweight Soft Mesh. My first ever surgery of any kind was a disaster that lasted three years plus the years after to heal from mesh removal So if you’re having mesh problems don’t let this account convince you to wait too long. You’ll know if things have any chance of getting better.
Also, finally, and maybe most importantly, Dr. Billing really does seem to know what he’s doing “in there”. If you’ve watched any videos of surgeons narrating what they’re doing and/or heard them describe it, there are all sorts of different ways that surgeons do things. There is no standard practice mesh removal method. As far as I know and according to his surgery notes, all that he did was carefully remove as much mesh as he could. No neurectomies were noted as having been done and I do not have any symptoms of neurectomy. No numbness or phantom pain. And no signs of recurrence.
So I can sincerely recommend seeking out Dr. Billing if you feel that you need to have mesh removed.
-
It’s good that you’re still improving. I thought everything was okay now since mesh removal, had no idea you still got discomfort. Hop in time it will go totally. I suppose the plus side is it’s a lot lot better than when the mesh was still there.
-
GI, that is great news. I too have found the judicious use of exercise to be noticeably therapeutic for “what ails me”. The human body is resilient and capable. Thanks for sharing your success story. It seems that what we focus on has a tendency to increase, so hearing good news can be very helpful.
-
I had been meaning to add an update to this Topic, but as often happens, I had a minor setback that made me reconsider. I like to deliver good news, not bad.
But, the good news now is that the setback has resolved. I have been slowly and steadily expanding my range of activities over the years, walking and running farther, and working harder, with pain/discomfort being the limiting factor. At this point in time, the area of the mesh implantation and removal is still my limiting factor. It’s the weak point.
The setback a few weeks ago was that I started to feel groin pain on both sides and pressure that made me think I might be having some sort of recurrence. This was after a week of rigorous hiking, running, walking long distances, and physical effort moving heavy boxes, along with taking up some contorted positions while working on various things. Normal active life stuff. After a week of resting with no real progress in minimizing the discomfort I went back to my old standby of trying new strenuous things to see if things got worse or better. They got better and I feel very good now.
So, the message is that after mesh removal it takes a long time for things to get closer to “normal”. This might be good news for anyone who’s having problems and bad news for anyone who’s having problems. I had the last piece removed in December of 2017 so it’s been about 5 1/2 years since then.
I went back and looked at my notes, basically a diary of daily physical activities, and found that in January of 2019, one year and a month after mesh removal, I had drafted a letter to Dr. Brown about hernia repair and removal of that last piece of mesh. That is the type of pain I was having at the time. I thought that I might have two indirect hernias and pain from the last piece of mesh. But, the pain and discomfort resolved and I moved on.
Over the next year my notes show that I had periods of strange feelings in the groins and lower abdomen, like tissues were stretching and things were breaking loose and moving around exposing new tissue/nerves, with feelings of pressure when sitting, but things continued to get better. Then there are about nine months of random observations but no significant reports of problems. My last entry was in October of 2020.
Anyway five years is a long time, plus the three years before the removal. Eight years and seven months since I went in for the walk-in walk-out mesh implantation at the Ambulatory Surgery Center that was supposed to make me bullet-proof. Over 10% of my life so far, at least.
I still recommend that people keep a diary or log of what they’re doing and what happens afterward. The strangeness of constant discomfort and occasional pain really affects your thought process and memory. It is a radical shift if you’ve been healthy up to the point of the hernia repair. I look back at my notes and realize that I would not remember much of what I had written. I might not realize the progress that I’ve made.
-
I replied to your message. One thing to be aware of is that mesh removal takes much longer than mesh implantation. So if you have somebody waiting for you make sure that they know that. It’s not the 45 minute in-and-out that implantation is.
-
@good-intentions thanks, will ask Billing on our next meeting before surgery.
-
I don’t know enough to say. I am not a medical expert and I don’t know anything about you except that you had two pieces of Bard 3D Max implanted for hernia repair. Nothing about your physical condition or how long you’ve had the mesh or what type your original hernias were.
I knew my own information and had the opportunity to decide “on-the-fly”. I drove 200 hundred miles two days after both explantations but I could have waited. Flying has its own issues though, with the pressure differentials. I don’t know anything about flying after abdominal surgery.
I would ask Dr. B. He has performed many surgeries of many different types. I am sure that he has had people flying soon after a procedure, whether they should or not. He would have the best advice.
-
How soon after surgery do you think is safe to fly back? I plan to stay up there for 3 days post Op.
-
Try the site’s message function if you want a private conversation. I share as little information as possible over the internet. I don’t know that I’ll have much to offer. I’ve had four surgeries under general anesthesia and they were all the same. Remove clothes, put on gown, go to sleep, wake up with no memory of what happened, surgery area hurts.
-
@good-intentions can you please shoot me an email? Need to ask you something privately if you don’t mind.
-
@good-intentions What was your experience when you arrived to see billing like beginning to end?
-
Forgot to ask was your mesh placed originally Laparoscopically like mine or was it an open surgery, don’t recall reading that in your post.
-
I think that I am the only person on the forum who had mesh removal by Dr. Billing. Many surgeons who do mesh removal laparoscopically do not attempt another repair. Most of them opt to wait and see if there is a recurrence. Often, apparently, the remaining tissue is stiff enough that there is no recurrence.
On the other hand, there are surgeons who will remove one piece of mesh and replace it with another, “just in case”. They might also perform neurectomies. There are people, some on this forum, who are stuck in a cycle of surgery after surgery, as one procedure leads to another.
In my case, Dr. Billing did not attempt another repair as he did not see any hernias, and he did not do any neurectomies. And I have been doing very well. But he spent much more time removing the mesh than many surgeons seem to do. Some surgeons are proud of how fast they can get in and get out. I think that that might be a reason for neurectomies. Easier and faster to cut the nerves than tease them off of the mesh.
If you have conversations with a surgeon make sure that you are prepared beforehand. Many of us will expect to remember all of out questions and be able to ask them once we get inside but once we get in to the doctor’s office, the doctor tends to run the conversation. You will leave the meeting with many unanswered questions if you don’t have a list before you start.
Also, many surgeons will get upset if you question what they plan to do. Despite all of the well-publicized problems with hernia repair many of them think that what they are doing is somehow different. Even though they are using the same methods and materials.
Good luck Ronnie. Keep detailed notes as you do your research. It can be very confusing especially when you’re suffering the pain. Don’t let my negativity dissuade you from your efforts. I’m just trying to shine a light on potential pitfalls.
Log in to reply.