
Mike M
Forum Replies Created
-
I am traveling in the next few days to have surgery with Dr. Kang in South Korea. http://gibbeum.com/main/main.php . He explains his procedure in the other threads but essentially it is similar to Bassini / Shouldice for direct hernias with smaller incision and a less “traumatic” procedure than Shouldice with equal or better results reported. Less tension too. Indirect Hernia the closest type of procedure would be the Marcy but it is not really a Marcy repair. All his procedures are known as his own Dr. Kang procedure.
If I did not discover Dr. Kang I would have reluctantly still been in the phase of “watchful waiting” with the Shouldice procedure and Dr. Grischkan being my #2. choice. I felt 100% comfortable with Dr. Grischkan but the Shouldice procedure is more involved but still with really good results.
I would never consider any other type of repair at my age other than an open tissue repair without mesh. I would only consider mesh as an option if I was 65+ or a couch potato. That isn’t to say mesh repairs are bad just not my preference. It is strictly a personal opinion based on what I have researched that it would not be in my best interest at my age. I am not a doctor so get a few opinions from actual doctors and testimonials from patients before you make up your mind imho.
If it means anything though – I never travel for anything other than traveling to another state for family vacation, occasional work obligations (I own a few companies and have to unfortunately), and recently this year for the Superbowl. I am not a travel person at all. Whatever is the opposite of travel person is me. Also having worked with medical professionals in my career (as a non-medical professional) at the highest level I am one of the most cynical people on the planet as it pertains to doctors.
tldr; Dr. Kang is the man.
-
So here is my thought process coupled with my experiences.
– Watchful waiting is probably bad imho. –
#1. It almost certainly will progress unless you limit your lifestyle. In my particular case it went from undetectable to hmmmm something is moving there slightly to pop oh I now have “moderate symptoms” all because of coughing from a minor cold. Obviously every case is different but recognize that it is a possibility it could progress quicker than you expect.
#2. Fixing it sooner usually results in a better outcome with less aggressive surgery being needed.
#3. There are MANY other serious symptoms that can occur and even potential damage other than just the “strangulation scenario” if it progresses. Nerve damage, cut off circulation to other “sensitive” areas vessels down there, tension, etc.
#4. It can progress to a serious point (even without strangulation) where other options you had for repair are no longer an option.
#5. Do you really want to be beholden to your hernia, walking on eggs shells, and ultimately on pins and needles trying to “manage” your hernia for an indeterminate amount of time? You have zero symptoms *now*. Understand that this can change unexpectedly and in a flash.
I took the “watchful waiting” stance at the beginning of Feb thinking it was no big deal. Hernia went from zero symptoms to moderate in a flash then back down to near zero symptoms. I wasn’t even doing anything out of the ordinary either and not even lifting weights.
You know what “watchful waiting” means to me?
The time it takes for me to do the necessary due diligence to find a doctor, procedure, staff, and hospital that best fits my needs.
-
I never had a “bulge” that you could see or even feel except when I coughed.
It feels like it is popping out to the left towards my upper thigh near the top of the hesselbach triangle when I cough then retracts immediately.
I am pretty sure when I was having “symptoms” it was lower than that spot which makes sense? I am speculating that laying down on my right side (opposite of the direction I felt the hernia was moving) allowed the hernia to retract or regress?
Who knows though it could have had nothing to do with it just really saw a dramatic change when I laid down on my right side 2 nights in a row.
I am babying myself until I get to Seoul and so far it is working! lol
-
Just in case it couldn’t be recovered this is what I remember –
“Cliff notes” version:
#1. Consider staying in the hospital (at least one night).
#2. Make sure you check to see if you have a “sliding hernia” type because it is possible to miss it via ultrasound on the first pass creating a reoccurrence.
#3. Most likely Prolene sutures were used (Dr. Kang uses these by default unless you request something else like absorb)
#4. Surgery went well and outcome was very positive.
Hopefully I didn’t miss anything. 🙂
-
Thanks William!
I am heading out soon and should be done with surgery sometime early next week.
Craziest thing started to happen about 2 weeks ago. I went from medium symptoms to nothing at all as of today. It all started when I started laying on my right side at night. I still know it’s there but it is 110% better.
Going to update as soon as I can when the operation is completed!
-
@Chuck
If it was me – I would go and get the most advanced detailed imaging (MRI or otherwise) of the region that is causing the pain. Based on your previous posts it sounds like it could be a urology related issue now. I would first have that imaging looked at by the best team of specialists I could find to see what they think. Then I would probably have what I deemed the 2nd best team I could find take a look at it for another guess.
I would go to a urology group at the Cleveland Clinic main campus in Cleveland, OH or maybe the Mayo Clinic in Rochester, Minn location. I am a little biased towards Cleveland because of the location and first hand experience with friends and family having “unknown” and “never before documented” problems resolved. One doctor at the Cleveland Clinic who solved and resolved my father’s liver issue completely is actually writing a book about my father’s case. This was after I took my Dad to countless specialists at other “top” hospitals . It was a gallbladder removal that lead to liver complications and nothing would resolve it. Long story not to digress.
You need to determine conclusively the benefit (if there is any) of mesh removal and that means seeing a specialist that can determine if it is causing your issue.
If it is somehow mesh related at all then I would consider talking to an expert in removing the mesh.
I know you had a bad experience with Dr. Grischkan but he is one of the foremost doctors regarding mesh removals and provided critical testimony in multiple lawsuits against the manufacturer of the Bard mesh.
You also have Dr. Yunis and of course my choice Dr. Kang who also wrote the book on mesh related issues overseas.
#1. Identify the problem or problems. Imagining, consulting the best related to that area of the body.
#2. Get a second or even a third opinion.
#3. Identify the best surgeon or surgeons that can resolve the problem.
I really would stress that if it was *me* I would unequivocally want *conclusive* scientific evidence backed by a medical expert in that field that it was the mesh and not another complication related to something else.
You do not want to make a bad problem worse when the underlying issue could be something else?
Get advanced imaging done and see a specialist asap! They may have to do another procedure (maybe a scope?) to go in and get a closer look too before they can determine the root cause(s) of your issue.
-
Sorry I did not mean to detract from absorbable *mesh*.
Here is some additional information / studies I found regarding that topic.
“https://pubmed.ncbi.nlm.nih.gov/28492358/”
tldr; “Results: The meta-analyses showed no difference in recurrence rates (median 18 months follow-up) and chronic pain rates (1 year follow-up) between absorbable- and permanent meshes. Crude chronic pain rates for the RCTs were 2.1% for the absorbable meshes and 7.6% for the permanent meshes. For the absorbable meshes, medial hernias were more susceptible for recurrence compared with lateral hernias ( P < .0005). None of the studies reported allergic reactions or other serious adverse events related to the absorbable mesh.
Conclusions: Patients with an absorbable mesh seem to have less chronic pain following inguinal hernia surgery compared with permanent meshes, without increased risk of recurrence.”
It appears the results are similar in this study to the open tissue absorb or not to absorb debate.
I would consult the leading mesh repair experts and take that into consideration.
If they believe the % increase is small then I would lean towards absorb.
I imagine the “recovery” time after surgery would be impacted since you want to give your body time to heal up completely before the mesh “dissipates”.
-
Here is some info I received from Dr. Kang when I inquired early on in this process. Note: This is regarding open tissue repair non-mesh.
“Polybutester and Prolene are non-absorbable materials and PDS (Polydioxanone) is an absorbable material.
I use Prolene in most patients but can use PDS if requested.
However, the possibility of recurrence can be slightly increased by 0.5-1%.
In Pure tissue repair, the length of the true material actually remaining in the body is less than 5cm.
The thickness is also very thin.
Therefore, I don’t think there is a possibility of causing problems even if this level of non-absorbable texture remains. ”
There have been some discussion of a 6 month threshold as the turning point to where your body has formed enough tissue to make up the strength of the repair?
Polybustester is polyester type material that Dr. Grischkan claims is the most inert however other commenters have indicated it could have a higher chance for inflammation since it is polyester. Dr. Grischkan uses the flexible polybutester suture to accommodate athletic movements. Athletes, powerlifters, etc. are a big piece of his clientele. Also Shouldice has a higher tension than other types of open tissue repair (desadara, Dr. Kang) so I can see where this makes sense.
Prolene seems to be the type informed patients on here prefer along with quite a few of the leading open-tissue repair doctors. I would like to see some reference material indicating as to “why”.
PDS – “Polydioxanone (PDS II) is a synthetic, absorbable, monofilament suture made from a polymer of paradioxanone (Figure 2). It has greater initial tensile strength than polyglycolic acid and polyglactin 910 but has the poorest knot security of all the synthetic absorbable sutures.24 The suture retains 74% of its tensile strength after 2 weeks, 50% after 4 weeks, and 25% after 6 weeks. There is minimal absorption by 90 days and absorption is not complete until 6–7 months after implantation.9 This retention of strength after implantation is an advantage over other synthetic absorbable sutures and is useful wherever extended approximation of tissues (up to 6 weeks), under tension, is required.35 PDS II is stiff and more difficult to handle than Dexon or Vicryl, but slides easily through tissue. PDS II was developed to improve the handling characteristics of the original form. It has low reactivity and maintains integrity in infected tissues and in urine and is often used in bladder surgery.36 Its long retention time may act as a nidus for calculus formation in patients with a history of urinary calculi. However, it is suitable for use in a wide variety of tissues.1”
Here are some studies between the absorb and non-absorb –
https://pubmed.ncbi.nlm.nih.gov/10365834/
tldr; “Results: Numbers of early complications were similar in the two groups; there were 2 wound infections in each. A total of 193 patients with 201 repairs had a documented follow-up (86%). There were 6 recurrences in the PDS group and 5 in the Prolene group, giving a total recurrence rate of 5%. This difference was not significant (Fisher’s exact test, p = 1.0).
Conclusion: Recurrence rates in both groups were higher than expected, but there was no difference between the two groups.”
Keep in mind this is from 1999 and the recurrence rates reported by the leading Shouldice facilities and doctors are 1% or lower per their data and “modified” techniques.
Here is an updated one: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400914/
“Results
Thirty-one trials were included (11,533 participants). No suture material reached the predetermined 90% probability threshold for determination of ‘best treatment’ for any outcome. Pairwise comparisons largely showed no differences between suture types for all outcomes measured. However, nylon demonstrated a reduction in the occurrence of incisional hernias with respect to two commonly used absorbable sutures: polyglycolic acid (odds ratio, OR 1.91; 95% confidence interval, CI, 1.01–3.63) and polyglyconate (OR 2.18; 95% CI 1.17–4.07).Conclusions
No suture type can be considered the ‘best treatment’ for the prevention of surgical site infection, hernia, wound dehiscence and sinus/fistula occurrence.”I am going take three things into account before I make my decision next week on PDS / Prolene.
#1. Surgeon recommendation based on my hernia, lifestyle, and anatomy.
#2. Recurrence chance based on #1. Example: Dr. Kang likes Prolene but will use PDS and tell you that there is a 0.5% – 1% chance increase of recurrence. I am assuming that is cumulative so that means you are closer to 1% – 2% overall when you factor in the procedure itself.
#3. Chance of complications later in life if non-absorb is used. This is sort of “pick your poison” between #2. and #3. Also I have zero concerns on “dangerous substances” being absorbed into the blood with PDS.
At the end of the day I think it is kind of splitting hairs as the listed references indicate.
Psychologically I think the edge goes to non-absorb of either type for me.
-
My understanding is the Muschaweck repair is limited to small hernias and there might be other specifics too.
-
I think you’re always going to have some sort of doctor check the results regardless for liability reasons.
However what would be interesting is AI interpreting a scan for hernias and suggesting the best possible repair method based on the damage and anatomy in the scan. Add probabilty and stats for things like pain and recurrence.
Maybe it could also recommend new and safer adjusted methods of repair.
I could see it turn into something amazing.
-
Mike M
MemberMarch 12, 2022 at 2:11 am in reply to: 25 Months since Dr. Brown permanently release my entire abdominal wallDr. Grishkan’s philosophy expressed to me was if the inguinal floor is damaged then the floor is damaged. I think he takes the position to fix everything so it is bulletproof.
Dr. Grischkan caters to a lot of powerlifters so maybe it makes sense.
I know if you have a small hernia there would be an option to not use the goretex repair with Dr. Grishkan.
I am debating which route to go regarding sutures. Absorbable, prolene, goretex, etc. I am pretty sure Dr. Kang can do all the above if requested. I guess when I finally see how big and bad my hernia is I will see what Dr. Kang recommends.
I dont weightlift as much as I used to but I do chop wood and toss 100lb logs around all day long in the summer “for fun” on one of my horse ranches. I also have to manipulate 2000lb+ Clydesdales when they get lively. Finally I am closer to 50 now than 40. Like GI mentioned I do have concerns as it relates to collagen rehab time regardless of any procedure.
I have had this hernia known for 6 weeks. Sometimes it comes after me in a blaze of glory and other times I just barely notice it is there. Either way 2 weeks from now it will be gone and hopefully for good.
-
Mike M
MemberMarch 9, 2022 at 10:05 pm in reply to: 25 Months since Dr. Brown permanently release my entire abdominal wallThat was one of my biggest questions.
Does the Cremaster still function after being cut / shaved / modified etc?
Cremaster is Skeletal muscle and when damaged these cells are stimulated to divide. The division process causes the cells to fuse with *existing* muscle fibers. The Muscle fibers regenerate and repair the damaged fibers.
The skeletal muscle fibers themselves, cannot divide *after birth. However, muscle fibers can lay down new protein and enlarge (hypertrophy).
So you have a few things at play here.
#1. If you take 30%-50% of the Cremaster you are causing some permanent damage in the sense the muscle fibers aren’t able to divide and just “poof” restore the muscle that is now missing. However the fibers that remain are getting a “work out” and can enlarge to potentially maintain the same muscle function as before because they will grow and increase in size / strength? At least as I understand it.
#2. Dr. Kang method appears to cause injury but he isn’t actually ***removing*** muscle tissue thus any damage incurred should be superficial. Skeletal muscle is designed to react and *HEAL* completely to the damage that Dr. Kang is causing in his procedure to the Cremaster muscle. At least how I understand it.
IMHO – “Cut through” and/or “Remove” healthy tissue / nerves, etc is a very very bad thing especially in this procedure.
It would be nice for one of the medical experts to chime in and correct me if needed and add input.
-
Mike M
MemberMarch 9, 2022 at 11:51 am in reply to: 25 Months since Dr. Brown permanently release my entire abdominal wallThe cremaster muscle is the thin fascial muscle of the spermatic cord made of skeletal muscle.
Indirect hernia you have to deal with it in terms of manipulating it more surgically (shaving possibly for a tighter repair) because it drops through the ring which is where the hernia occurs? Dr. Kang and Dr. Yunis have another method that avoids this potentially unfortunate step? None of the doctors I spoke to including Dr. Grischkan cut any nerves. Dr. Yunis had stated to another member that “no one does that anymore?” but I am sure some still do. Perhaps the Shouldice Hospital?
One of the members on here had it down at the Shouldice Hospital and stated he didn’t realize they did that or know a difference before/after?
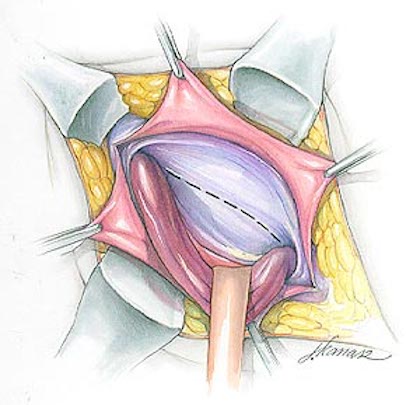
If the procedure only deals with direct I would think it just needs to be moved out of the way as illustrated.
-
Does “gurgling” near the hernia site really mean it’s incarcerated though?
I understand it is a cause for concern but it seems to be this is one of those “check engine” light symptoms to some degree.
I feel gurgling at my hernia but was diagnosed with non-incarcerated hernia (no imaging only physical exam) but with other symptoms (i.e. minor dull pain / pressure). I can’t feel a single thing sticking out unless I cough even then it pops out and pops back in again.
I think we all have felt gurgling in our stomachs and our digestive track in general throughout our lives.
That doesn’t mean there is a breach in each one of those spots?
If you have a hernia you are going to have a breech that will easily transfer pressure and sound through that cavity / weak spot to the surface.
It is going to be very thin / weak in the spot.
-
Mike M
MemberMarch 9, 2022 at 10:29 am in reply to: 25 Months since Dr. Brown permanently release my entire abdominal wallFirst let me say I am very sorry to hear that this happened to you and I hope you can find someone to resolve your problems long term.
@Herniatalk Community Regarding “dissect” the spermatic cord w/ open tissue repair.
Doesn’t almost every open tissue repair require this procedure and it simply means you are carefully moving the cord out of the field of surgery for direct hernias moving it back in place once it is completed?
I assume this is to prevent damage during the actual repair of the hernia itself?
-
@Watchful – My take on Dr. Kang cremaster response is two things.
#1. Direct Hernia the cremaster is not directly involved in his repair and will not be modified.
#2. Indirect Hernia he will also work with extreme care however it will need to “manipulated” to an extent as to fix the issues with the indirect hernia with his procedure. The expectation is there could be some damage but it will be “superficial” and not affect the outcome. I don’t know if you could ask for anything more with any type of open tissue non-mesh repair.
In regards to Dr. Kang using a “non standard and not well known procedure”. This is an excellent point. However it is my understanding after posing this question that Dr. Kang uses modified versions of existing well-known procedures. The modifications are his version of improvements.
Indirect – The repair method (at least the ideology) is similar to a Marcy? https://www.sportshernia.com/marcy-technique-nonmesh-hernia-repair/
Direct – It is similar to Bassini / Shouldice repair.
You always have to take into consideration for the law of unintended consequences anytime a standard procedure is “modified” to improve it especially to the extent that it resembles a new procedure rather than the original.
I took questions from people that researched the topic extensively, feedback from other doctors, my own questions and ultimately accepted the responses. I will probably keep asking questions up until the knife starts slicing. lol
Everything I have research so far from Dr. Kang is very conservative in his methodologies, approach, and his appreciation for keeping nerves, muscles, etc. “intact”.
So conservative to the point where I ask myself is it a lot more likely for a recurrence to happen 10-20 years down the road using this method vs. anything else in my 40 something but active age group. I am not sweating a 1% point however which seems to be where the data leads.
Dr. Grischkan and Dr. Kang have been extremely successful in working on a wide range of body types, athletes, body builders, martial artists, people with pre-existing conditions, extreme cases etc. so my case should be a walk in the park. Crossing fingers.
@Good Intentions – 100% Agree. Dr. Grischkan’s “modified” Shouldice is enough of a comprise I could live with with if I had to in a pinch with all of the other checkboxes marked.
I do not have enough data with Dr. Yunis to tell you if he would be able to meet my criteria because I never got a chance to speak to the doctor directly. Based on other patient positives experiences it does seem like he would be able to meet all criteria with the one asterisk you mentioned. Dr. Grischkan proposed a very simple and easy work around which was totally acceptable as did Dr. Kang. I am concluding for now that my experience with Dr. Yunis was more related to a specific staff member / assistant which I found to be appallingly devoid of compassion and totally unprofessional as it relates to male patients. The request was posed in a very polite and benign manner and the response was power trippy, incredibly “weird”, and not something I am comfortable with in quoting verbatim. Not to be dramatic but I mentioned it to my wife just to make sure there wasn’t something I missed or another way I could take it and she was taken back by it. I suspect (although unknown) Dr. Yunis would have been able to make simple and agreeable accommodations if I had spoken with him directly.
-
I plan on going to Dr. Kang the 1st or 2nd week of April.
If for some reason my condition changes unexpectedly and dramatically then I will go to Dr. Grischkan. There is zero chance I would choose the Shouldice Hospital in Canada over Dr. Grisckhan.
Desarda repair had too many concerns from experienced members including some nightmare stories for me to consider it as an option.
Dr. Conze in Munich sounded good but it is my understanding that the muschaweck repair is very specific and for small hernias exclusively. Not sure what I have at the moment. Also a lot of concerns about the cremaster in their procedures. However it is my understanding that the Munich Hospital is very careful regarding nerves and images nerves route specifically? to avoid long term issues.
Dr. Yunis works around the cremaster muscle and is a vascular surgeon which is a plus in my book. ThunderRose had success in having him agree to perform the procedure with some of her requirements. However Dr. Yunis does not complete as many open tissue repairs as the other experts and I recently read a story of a patient requiring a bag after one of his operations.
Here is my checklist by rank of importance.
#1. Surgeon experience and skill specifically in the procedure performed.
#2. Type of surgery – No-Mesh (or minimal if absolutely required), open tissue repair under local or twilight sedition. I also used the checklist by ThunderRose as a basic guide along with some understanding of the procedure.
#3. Longevity – I will sacrifice a slightly higher chance for reoccurrence if it means avoiding a large piece of mesh. I disagree that this is an Airplane to Cars analogy in terms of risk vs. reward. I do agree that there is a higher chance for reoccurrence especially in large hernias with older patients without some mesh type structure to assist. I will roll the dice on this one and hope for the best.
#4. Bedside manner, ability to meet basic, reasonable, and *respectful* accommodations for a patients needs, ability for staff and the Doctor to communicate in a healthy and respectful manner to patients. Tied for #1 for me for non-emergency situations.
#5. Specialized Outpatient facility for Hernia Repairs – Not huge but has perks.
Choices:
Open non-mesh – #1. Dr. Kang and #2. Dr. Grischkan (mainly because of the cremaster concern)
All other options – #1. Cleveland Clinic expert (there are a few really good ones up there) or Dr. Towfigh possibly. Had I known I had a hernia when I was in Bev Hills for the Superbowl I would have extended my stay to see Dr. Towfigh for another opinion.
-
@Watchful – Regarding cremaster shaving – Dr. Grischkan did not give me the option. Dr. Grischkan stated that it would be incredibly difficult to get a tight repair in that area without doing something. “tight repair” as in one he would be comfortable with in long term. I could probably force the issue but I would hate being the first one for him to test it on if that is what he does and has experience in doing without complications.
Dr. Grischkan repairs the entire Inguinal floor regardless of indirect or direct where as Dr. Kang has a tailored approach. Dr. Kang will add more support depending on the circumstances and repair everything if it is needed. Repairing everything regardless of circumstance is definitely more involved but I guess it gives you the added reassurance that you won’t get an indirect hernia later down the road if you had a direct hernia? at least that was the impression I had when it was explained to me.
Dr. Kang does *not* cut any nerves and leaves everything intact.
Regarding Dr. Kang and cremaster this is how it was explained to me by his team whereas the cremaster is the warehouse.
Dr. Kang – “To repair the facilities in the warehouse, you can think of it as if you had to open the warehouse door and enter it, split open the master muscle fiber, operate on the structure inside, and close the warehouse door again.”
Dr. Kang – “I do not remove or damage whatever inside body structure. Only in the type/case of ‘indirect’ hernia, along the fiber plane of cremaster muscle, after I split and I need to deal with the sac in there, I might incur a little bit of damage inevitably but it is almost ignorable. ”
In my opinion that is a lot better than taking or taking up to 50% of the cremaster.
@William Byrant – I did speak with Dr. Yunis’ assistant / gatekeeper in an attempt to setup a consult. However it did not get past the initial stages as I was taken back by the lack of empathy and professionalism by that individual when I made a simple inquiry and request regarding their procedure and accommodations. Dr. Kang, Dr. Grischkan, and all the other doctors I consulted have been incredibly compassionate and understanding throughout the entire process.
Dr. Yunis has an overwhelming amount of positive reviews and is a vascular specialist. That can’t hurt? I also understand he works around the cremaster muscle completely which is great.
Some negatives reading the forums here regarding Dr. Yunis. #1. Someone stated a patient ended up having to have a bag with one of his procedures after nicking a bowel? I suppose when you do thousands of repairs there are bound to be some complications on some of the patients. You just hope that % is incredibly small. #2. His primary preference and specialty? method of repair is not tissue, it is mesh.
Ultimately it is really up to Doctors themselves in regards to how things are going to be setup and handled so my advice is if Yunis is a consideration for you make sure you speak to him directly before you form a final opinion.
-
Just a little follow up – I met with Dr. Grischkan and it was a very positive experience. I found Dr. Grischkan to have an excellent bedside manner and he was very knowledgeable. He showed me examples of some difficult cases he worked on (which mine is not) with very positive outcomes. Additionally he had a lot past and very recent of personal experiences expressed in hand written letters / cards attach to the wall as soon as you walk in making you feel a little more at ease.
He also tailors the procedure depending on the size, scope, and anatomy of the patient. If it is a seriously large hernia his approach is very aggressive with the polybutester suture that has demonstrated to be one of the best inert options available.
Dr. Grischkan also does not cut any nerves but he does trim the Cremaster muscle 30%-50%.
The entire procedure as explained to me checked off all my boxes except for the Cremaster portion. I would rather have someone work around it and risk a little higher reoccurrence then trim it.
Ultimately I think I will try Dr. Kang. There are an overwhelming amount of positive testimonials, he is extremely well respected, and his credentials are impeccable from what I have found.
Most likely I will opt to stay in the hospital for an extra day if needed to make sure the sutures are 100% solid before I go back to the hotel.
I think the pure tissue repair method is an interesting study on whether or not the human body can handle a more “natural” tissue repair in that area without requiring synthetic assistance. I guess time will tell.
I did consider the more “traditional” mesh repair method using a specialist from the Cleveland Clinic but I would rather avoid general and an hour long surgery if possible.
-
Mike M
MemberMarch 11, 2022 at 3:28 pm in reply to: 25 Months since Dr. Brown permanently release my entire abdominal wall@MarkT – The vast number of successful and documented repairs of Shouldice (and modified) is the biggest selling point. Follow up from you and others that have experienced it with success (including no loss of cremaster function) is a testament that there are other viable options out there besides the status quo mesh mesh mesh.
I think the point to being so hyper focused on one aspect or another for a particular procedure is solve these concerns. Can we dismiss it ? or it is really an issue? There is a lot of mixed opinions so the more successful input the better.
I have a lot of respect for surgeons like Dr. Kang, Dr. Grischkan, and Dr. Yunis who continue to modify and improve sound methods by reducing the amount of the nerves, tissue, and overall area impacted.
It is my understanding that Drtowfigh has also created innovations and vast improvements for the mesh procedures that she performs?
I think mesh has its place too. If I was 65+ or had a pre-existing condition (connective tissue disorder like marfans? perhaps) someone could probably convince me to pick mesh over an open tissue repair. There have been countless numbers of “successful” mesh repairs without issue. I am not a fan of it because of how the operation is performed and the underlying requirement of mesh to ultimately solve the problem at my age. Since there are other viable options available I will pick just about any other route.
@Good Intentions – Outside of the usual negative stories of mesh it is interesting to get more details regarding of what mesh modifies / interacts with in that area. I wonder how the other open “pure tissue repair” materials break down and/or interact with that area over time. There seems to be a lot of material options open tissue repair doctors use from flexible gore-tex to ones that dissolve over time.
