Good intentions
Forum Replies Created
-
Good intentions
MemberOctober 24, 2025 at 11:51 am in reply to: Testicle/Spermatic Cord Pain Post-ShouldiceAt this point, so early after surgery, there’s probably nothing that can be done. It’s too soon.
Many surgeons have “modified” the Shouldice procedure. Some even implant mesh and call what they did a modified Shouldice procedure. There are two-layer and four-layer Shouldice procedures. Not the same thing.
It would be interesting to learn what your surgeon actually did and why they call it a Shouldice-type procedure.
Good luck.
-
Good intentions
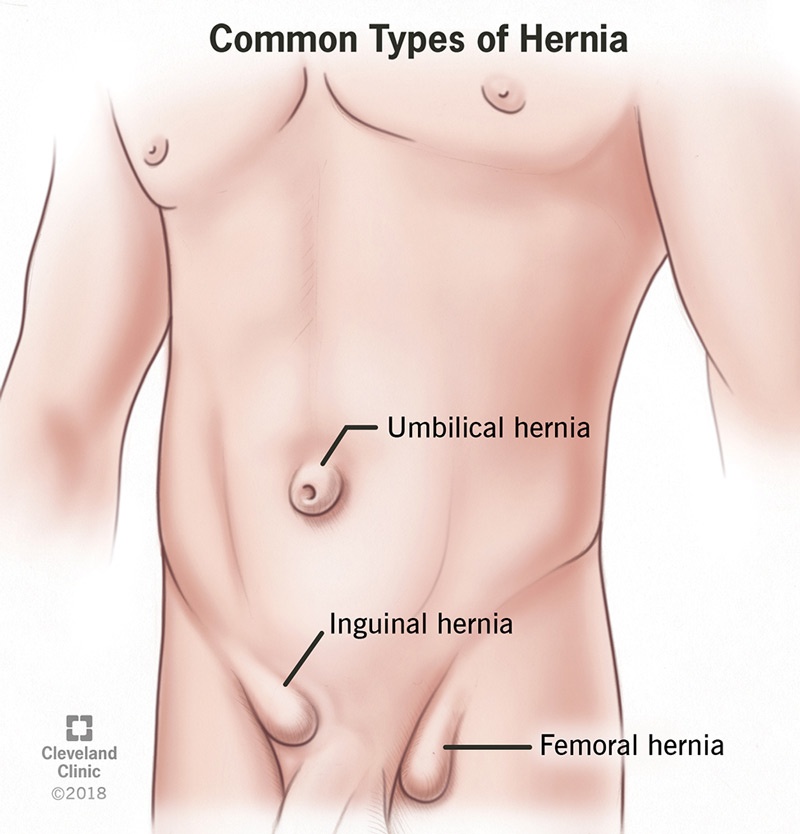
MemberAugust 25, 2025 at 4:27 pm in reply to: Recurrent hernia repair of complex herniaJust curiosity, but how do you know that you have a recurrence? Pain, a lump, material where it’s not supposed to be? And why did you call it a complex hernia? The PHS is used for typical inguinal hernias.
Also, just an opinion, but I don’t think that Dr. Towfigh can tell you why the other surgeons had their opinions. It’s the chaotic nature of hernia repair today. A big complicated mess of materials and methods. None seemingly better than others. The one that’s been called the worst, the plug, is the most popular. I think that most surgeons just learn one method and that’s what they do.
Basically, what Dr. Towfigh suggested was that you should choose a TAPP surgeon. The advice about trusting your surgeon only seems valid if you choose the right one. You trusted the one that did the PHS and now, apparently, you have a recurrence.
Good luck. You seem aware of the various pitfalls. You’re about ready to just create a checklist and use a process of elimination to choose one.
-
Good intentions
MemberAugust 24, 2025 at 9:37 pm in reply to: Recurrent hernia repair of complex herniaIt will probably help your decison-making to fully understand the Prolene Hernia System. When complete you will have a piece of mesh between the peritoneum and the abdominal wall, like a TAPP or TEP procedure, connected to a piece of mesh in the inguinal canal, like a Lichtenstein procedure.
You also need to fully understand what yoru surgeon meant by “recurrence”. Literally, it means that the same hernia that was present before has come back. But, I think that the word is sometimes used if any type of hernia appears after a hernia repair.
If the hernia has recurred around the mesh that was placed before then some or all of the mesh will probably need to be removed. If it’s a new hernia in a different place then the solution will be different.
Here’s an image of the PHS, and a description of the method of placement.
https://cobalt.pipelinemedical.com/Product/Detail/system-hernia-medium-prolene-3-cm-34571
cobalt.pipelinemedical.com
Systems: Prolene Hernia System, Medium, 3 cm | Pipeline Medical
The PROLENE™ (Polypropylene) Hernia System is a sterile, pre-shaped, three dimensional device constructed of an onlay patch connected by a mesh cylind
-
Here are some of the old threads about Gibbeum Hospital.
https://herniatalk.com/forums/topic/dr-kang-gibbeum-hospital-stephen-kwon-and-more-review/
https://herniatalk.com/forums/topic/non-mesh-with-dr-kang-in-korea-journal-updates/
-
Finally, since you’re on the west coast apparently, Dr. Kang of the Gibbeum Hospital might be worth a look. That is where I woudl go if I had a recurrence. People say that the experience is easier than expected, despite the language difficulties. You can find instructions on the forum with detailed suggestions.
https://gibbeum.com/main/main.php
-
Here is Dr. Brown’s web site. His practice was acquired by Dr. Nguyen. Dr. Nguyen did not change much on the web site, so it’s not clear what type of repair he uses. I think that I’ve seen that he likes the absorbable meshes, but the web site still shows no-mesh repair.
I don’t know if the reference to Dr. Nguyen in Los Altos refers to the Dr. Nguyen in Los Gatos.
https://herniatalk.com/forums/topic/hernia-surgeons-using-phasix/
-
Dr. Billing might. He mentioned that he would do a no-mesh repair for me if I had a recurrence after mesh removal (I have not, since removal seven+ years ago). Apparently he does robotic surgery now. I have not corresponded with him since about five years ago. He does not advertise much for hernia repair but he does do them and he has a word-of-mouth reputation for mesh removal. He is a great guy, definitely worth contacting. He is in the Seattle area of Washington.
https://www.transformweightloss.com/meet-our-team/
https://www.transformweightloss.com/weight-loss-solutions/hernia/
-
I occasionally will feel a twinge in the groin area if abdominal pressure increases. This is after mesh removal..
You need to find a surgeon that removes mesh, probably at a hernia repair specialization practice. They will have heard similar symptoms and will know the before and after of mesh removal. Medical care is very silo’ed today. Good luck.
https://www.centerforherniarepair.com/removal-of-mesh-from-previous-hernia-repair/
centerforherniarepair.com
Removal of Mesh from Previous Hernia Repair - Center for Hernia Repair Sarasota
We offer safe hernia mesh removal options for those experiencing pain and discomfort from hernia mesh. See how our experienced surgeon can help you.
-
The range of the lawsuits is expanding to newer meshes, from recent surgeries. Here is one against Becton Dickinson regarding Bard 3D Max Light mesh, called out specifically. Even if the plugs disappear, the others are still out there. Fascinating to see how these new suits will be handled. 2023 is not even two years behind us. The latest and greatest methods were available. What went wrong? How will the word “defective” be defined?
“May 15, 2025: California Man Seeks Settlement in Federal Hernia Mesh Lawsuit
Gerald Lee Wheeler of California has filed a hernia mesh lawsuit against C.R. Bard and Davol, the companies that manufactured 3DMax Light Mesh and Perfix Plug. Gerald had these two devices implanted in 2015 and 2023; however, he experienced complications from these defective products and had to have corrective surgery. He is requesting a full jury trial on all of his allegations and asking for a fair settlement package.”
https://www.robertkinglawfirm.com/personal-injury/hernia-mesh-lawsuit/hernia-mesh-settlements/
-
Typical clinic page, from a very well-known clinic. At least they provide a number, although it is buried at the end. 10% chance of chronic pain.
https://my.clevelandclinic.org/health/diseases/15757-hernia#management-and-treatment
“What are the possible side effects or complications of the treatment?
There’s a small risk of general surgical complications, such as excessive bleeding, wound infection or reactions to the anesthesia. Some people have difficulty urinating for a short time after surgery. About 10% of people report chronic groin pain after inguinal hernia repair, possibly due to nerve damage.”
-
The FDA site, currently.
https://www.fda.gov/medical-devices/implants-and-prosthetics/surgical-mesh-used-hernia-repair
-
Good intentions
MemberMay 10, 2025 at 5:25 pm in reply to: The News Feed page seems to be locked up. No posts allowed. But Discusssions woThe main page will also not accept comments. Maybe why nobody has replied to the last person who asked for help from the forum. Disappointing for them, I’m sure.
-
Good intentions
MemberMay 10, 2025 at 5:21 pm in reply to: The News Feed page seems to be locked up. No posts allowed. But Discusssions woIt uploaded the image as a document but would not upload it as a picture. Oh well.
The image shows what happens when a person tries to post on the main page.
-
Good intentions
MemberMay 10, 2025 at 5:19 pm in reply to: The News Feed page seems to be locked up. No posts allowed. But Discusssions woI tried to load an image and it failed. Maybe this will work.
-
Realized a minor milestone today. I can wear my old 34 inch waist shorts without pain or discomfort. I had almost given them away since even a 36 inch waist had been uncomfortable. I never thought that my abdomen, the mesh damage zone, would feel right again.
The list of little tricks I developed over the years have all helped. I’ve increased the level of exertion in my exercise and the duration and have taken up running again. The consistent progress, although taking years, shows that it was the mesh that did most of the damage. My abdominal wall seemed to have thickened, and the remnant of mesh that was left behind was still causing pain and localized inflammation. I can still feel it at times but it doesn’t seem to affect as large of an area as it did.
Posting for anyone that is still trying to recover from mesh removal. If things got bad enough to have the mesh removed then the damage that was caused will probably take years to heal and readjust. Don’t lose hope. Just keep working at it. It really is a shame that the community of surgeons has given up trying to find a better hernia repair method.
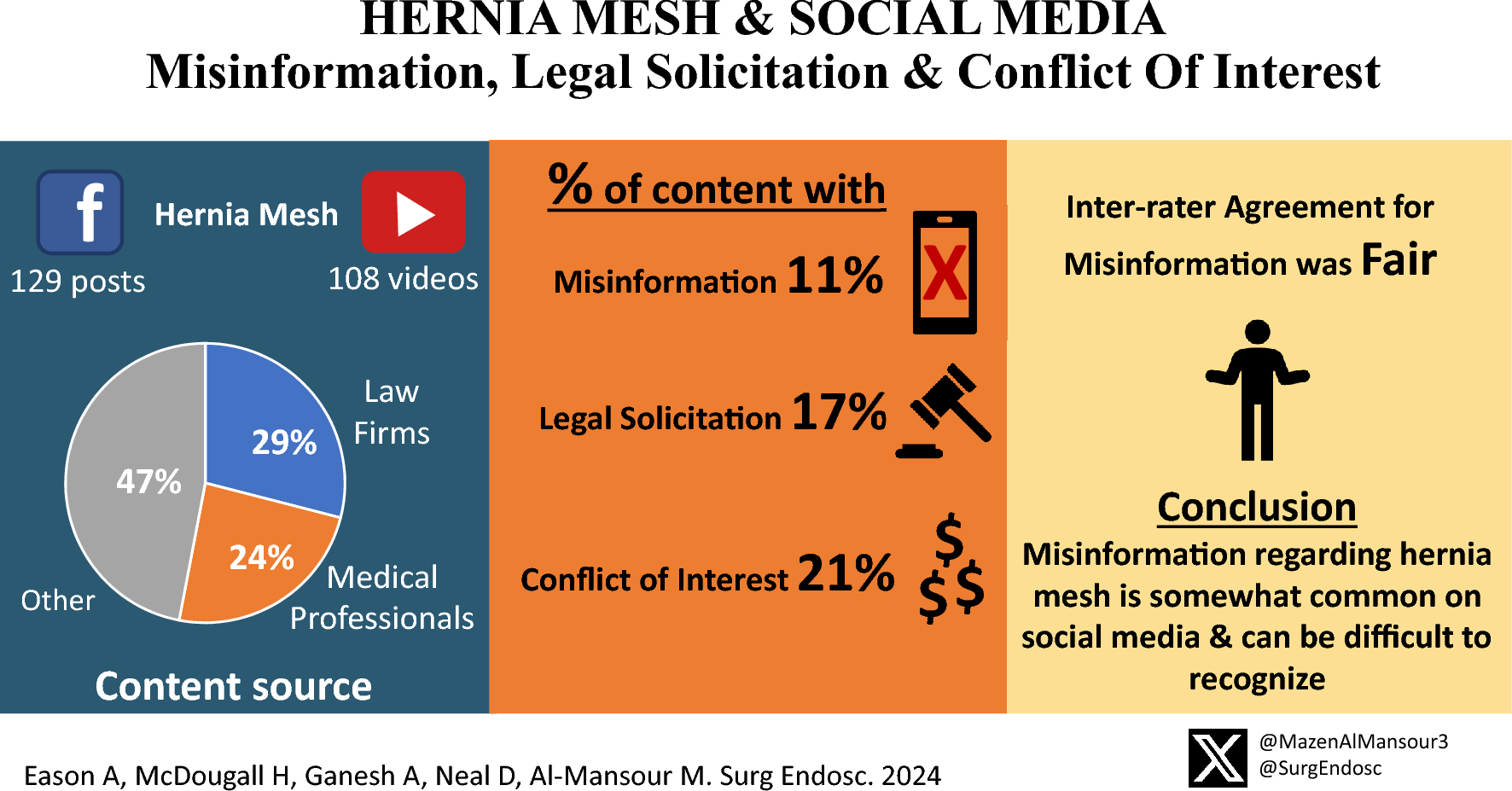
But the gaslighting, or outright ignorance, continues. It’s pretty amazing.
https://link.springer.com/article/10.1007/s00464-024-11320-w
link.springer.com
Background Patients often utilize social media platforms as a resource for medical information. Lately, hernia mesh has been surrounded by controversy due to highly publicized mesh recalls. We aimed to assess the rates of misinformation, legal solicitation, and conflict of … Continue reading
-
https://www.balancedbridge.com/bard-hernia-mesh-2025-updates/
“What does this mean? Again, we cannot know for sure how much the final settlement in the Bard Hernia Mesh MDL is going to total, but with legal fees and the settlement amount, it appears to be near $2 billion.
Something else to know is that this will not be the end of hernia mesh lawsuits. It is unlikely this will even be the end of hernia mesh lawsuits for Bard. Other individuals are still pursuing litigation on their own.
In addition, hernia mesh lawsuits are just now ramping up for other makers of hernia mesh products like Covidien, which now has 1,500 people in its MDL.
The bottom line is, people who have been involved in the long battle of Bard Hernia Mesh products are finally getting close to receiving compensation as the result of their injuries.”
-
It’s been 6 weeks. You’d still be in the mesh/tissue ingrowth and shrinkage phase. Your expectations for immediate return to pain-free action seem way too high but, on the other hand, that is what the typical patient is sold. No surgeon will be doing any surgical procedures on you at just 6 weeks.
And that that space you’re talking about is called the perineum. You’ve probably seen pharma ads about perinum inflammation/pain being a side-effect of various drugs.
Also, it’s pudendal nerve, not pudenal.
Good luck. Wait and don’t overdo things and you might come out okay in the long run.
-
It would depend on the type and size of hernia. I’d probably start over with researching what the various surgeons are doing these days. There are surgeons out there, not well known, like Todd Ponsky, who uses a non-mesh technique for indirect hernias. His specialty is pediatric surgery but he has repaired adults. He would probably also know of the various non-mesh techniques since he is not married to mesh like most of today’s surgeons.
It’s still a major challenge to make the choice. Surgeons have given up trying to find a better repair method. Their focus is on speed of the procedure and disclosure, to displace liability. Mesh has taken complete control. The device makers have shouldered the burden of the lawsuits, since they have the money for the lawyers. Surgeons don’t have to worry about that aspect anymore as long as the disclosure forms get signed. And as they look around they see that “everybody is doing it” so it feels okay to use mesh on everyone. It’s the “best” that is available to them, even though they know that it’s not really good enough.
My cynicism has not diminished. The mesh situation blends in with much of what is happening in society today. There’s still hope though. You just have to put in a lot of effort.
Honestly, I would go to South Korea to have any hernia repaired. Dr. Kang uses a “tailored” approach, apparently,, meaning that he assesses each hernia individually, and applies what he believes to be the best method of repair for that situation. Even Shouldice surgeons uses a conveyor belt type approach, as I understand things. Each repair is the same, and meant to do more than just repair the hernia that they see, but also to prevent any type of future hernia. They do more than is necessary, from what I’ve read.
Make sure that you get a good consultation before you make a decision. Unfortunately, surgeons have to “make the sale” in order to keep their practices going so it might be hard to get an honest opinion without offending, plus a typical consultation only pays 15 minutes to the surgeon if it’s billed to insurance. Not much time answer your questions so take a written list with you. And take charge of the conversation. It will probably be uncomfortable. I wish that I had a more straighforward answer. Good luck.
-
Good intentions
MemberMay 17, 2025 at 1:04 pm in reply to: Seeking recommendations for non-mesh surgeons — Runner’s dilemmaThanks for the update. There are very few true-to-life places on the internet where people can get good information.
Unfortunately, the HerniaTalk forum seems to be broken at the moment and only people who have created an account, signed in, and moved to the Discussion area, can respond. The main NewsFeed page is broken and not accepting posts.
Good luck and happy that you made it through the minefield.
@drtowfigh notifying Dr. Towfigh in case she doesn’t realize the NewsFeed is broken. She did post on the forum after I posted about it days ago. But maybe she missed my message. Or it might be that one of her assistants only logs in to post links to the YouTube page and nobody is actually monitoring the forum. Who knows.
-
Good intentions
MemberFebruary 24, 2025 at 6:35 pm in reply to: Argentine footballer has inguinal hernia repairedI had most of two pieces of Bard SoftMesh removed in late 2017. It was originally implanted in late 2014 for repair of a right-side direct hernia. The surgeon said that he found something on the left side so he did it also. It’s not uncommon, bilateral mesh implantation is popular in the hernia repair field.
A small piece of mesh was left behind on the right side during explantation because it was too entangled with the critical structures of the spermatic cord. It has been an irritant for years, sometimes severe, but has become more of just a mild annoyance over the last couple of years. Sometimes I feel very good and healthy, other times I feel the soreness of the mesh irritation and re-realize that I have not returned to full health. I still carry some of the burden of mesh-based hernia repair.
You can follow the publications in Hernia Journal and see that very little progress has been made in solving the problems with mesh. New studies of the same old problems. The materials have not changed at all.
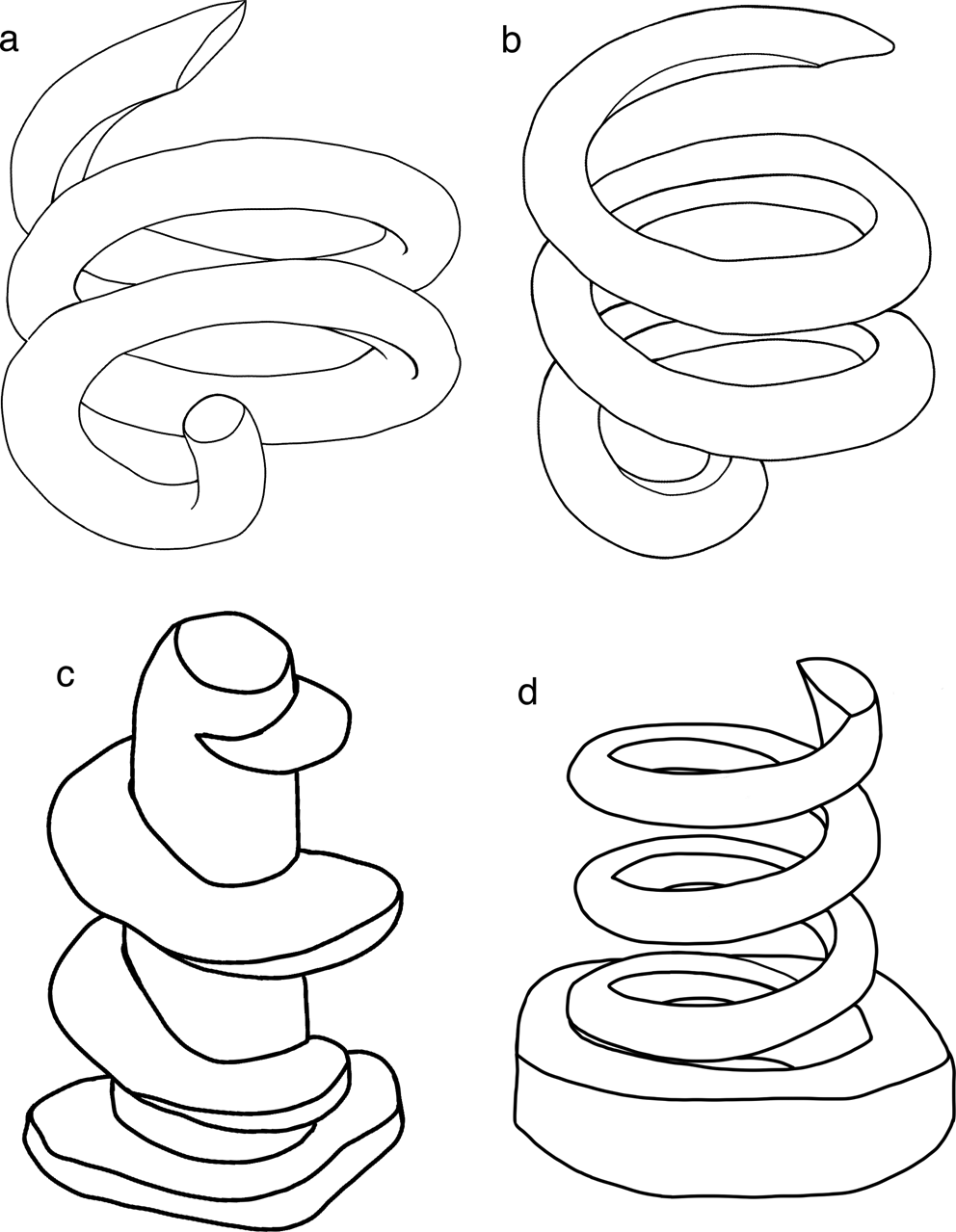
Here is a new study of fixation methods. The information available to the surgeons to make better decisions is poor. And access to data is typically hidden behind a paywall.
https://link.springer.com/article/10.1007/s10029-025-03276-0
Hernia Article
Mesh fixation in laparoscopic groin hernia repair: a comprehensive review of techniques and devices
Review
Published: 19 February 2025
Volume 29, article number 105, (2025)
Patricia Rancke-Madsen, Stina Öberg & Jacob Rosenberg
Purpose
Laparoscopic groin hernia repair has increased in popularity in recent years. Many laparoscopic mesh fixation techniques and devices are available, but there is a lack of high-certainty evidence favoring one fixation technique over another. This narrative review aimed to provide a comprehensive summary detailing the available mesh fixation techniques and devices used in laparoscopic groin hernia repair.
link.springer.com
Purpose Laparoscopic groin hernia repair has increased in popularity in recent years. Many laparoscopic mesh fixation techniques and devices are available, but there is a lack of high-certainty evidence favoring one fixation technique over another. This narrative review aimed to … Continue reading